
Building a Stronger Behavioral Health Workforce for NY’s Children and Ending the Waitlist Crisis
Testimony & Public Comments
February 4, 2026
On Wednesday, February 4, Associate Executive Director of Data and Policy Alice Bufkin submitted testimony for a FY 2027 Joint Legislative Budget Hearing with state leaders on Mental Hygiene. This testimony dives into data on New York’s youth mental and behavioral health waitlist crisis, with severe workforce shortages and low reimbursement rates leaving most providers unable to meet demand and only 1 in 4 Medicaid-enrolled children receiving the services they need. As a leader in the Healthy Minds, Healthy Kids Campaign (HMHK), CCC recommends a $200 million investment to strengthen rates and expand the workforce and calls for removing behavioral health services from Medicaid managed care to reduce administrative barriers and reinvest funds into services.
Read the testimony below.
Testimony of Alice Bufkin
Associate Executive Director of Data and Policy
Citizens’ Committee for Children of New York
Submitted to the New York State FY 2027 Joint Legislative Budget Hearing
Mental Hygiene
February 4, 2026
For 80 years, Citizens’ Committee for Children of New York (CCC) has been an independent voice for children advancing child and family well-being through research, advocacy, and civic engagement. With deep expertise in data, policy and child-serving systems, CCC champions proven solutions and mobilizes allies to secure reforms that improve child outcomes and promote equity. CCC drives systems change to ensure every child is healthy, housed, educated, and safe.
CCC also coordinates the Healthy Minds, Healthy Kids Campaign (HMHK), a statewide coalition committed to ensuring all children in New York have access to the high-quality behavioral health services they need. Through this coalition, we work directly with parents, young people, advocates, and providers throughout the state who have witnessed firsthand the harms of a behavioral health system that has failed to serve the children, youth, and families who most need care.
Thank you, Chair Pretlow, Chair Krueger, Chair Brouk, Chair Simon, and members of the Senate and Assembly Committees for holding today’s Joint Hearing and allowing us the opportunity to uplift key challenges and recommendations for enhancing access to children’s behavioral health services in the SFY 2026-27 Budget.
A Children’s Workforce in Crisis
For years, providers and families throughout the state have uplifted the widespread inability of children and families to access timely mental health and substance use disorder (SUD) supports. To understand the depth of the waitlist crisis confronting children and families in the state, CCC and partners in the Healthy Minds, Healthy Kids Campaign conducted a survey in the Fall of 2024 of children’s outpatient providers across the state.[i] We received a total of 43 responses representing Long Island, New York City, Mid-Hudson, Capital District, Mohawk Valley, Southern Tier, Western New York, Finger Lakes, Central New York, and the North Country (Empire State Development Regions). Provider types included the following children’s outpatient services:
- Article 31 Outpatient Clinics (22 responses)
- Children and Family Treatment and Support Services (CFTSS) Therapeutic Services: Psychosocial Rehabilitation Services (PSR), Other Licensed Professional (OLP), and Community Psychiatric Supports and Treatment (CPST) (27 responses)
- CFTSS Peer Services: Family Peer Support Services (FPSS) and Youth Peer Support (YPS) (18 responses)
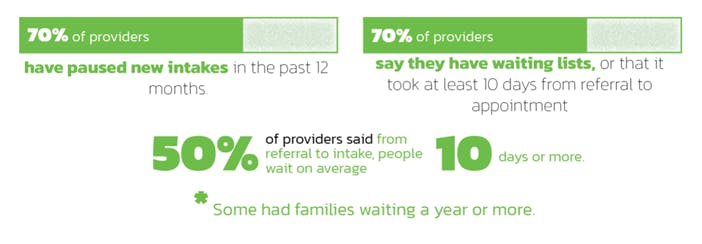
These responses indicate striking and widespread waitlists and delays in care. All program types rated barriers such as inadequate reimbursement, staff turnover, and staff vacancy as significant, while CFTSS program types also nearly unanimously identified inadequate reimbursement for travel, care coordination, and documentation barriers as significant.
A majority of OMH Article 31 Clinics report children and families waiting for services:

A majority of OMH CFTSS therapeutic services (Psychosocial Rehabilitation, Other Licensed Practitioner, Community Psychiatric Supports and Treatment) report children and families waiting for services:

A majority of OMH CFTSS Peer Services (Family Peer Support Services, Youth Peer Supports) report children and families waiting for services:
The Impact of Workforce Shortages on Children and Families
This data could not be more clear: providers do not have the capacity to serve the number of children who need care, and as a result families are sitting on waitlists for weeks, months, and even years to get the care they need. In fact, a 2024 study by the Healthy Minds, Healthy Kids Campaign found that at most, 1 in 4 New York children covered by Medicaid are accessing the outpatient behavioral health (mental health and/or substance use disorder) services they need.[ii]
3 in 4 New York State Children Who Need Behavioral Health Care Are Not Receiving Critical Services

Unfortunately, chronically low reimbursement rates have contributed to massive staff turnover and vacancies, and widespread provider shortages. HMHK found that an additional 6,281 providers are needed to address the outpatient workforce shortage. This includes:

These shortages are, in turn, leading to unacceptably long waitlists for services. As a result of this waitlist crisis, families across the state are experiencing hospitalizations, police involvement, lost education, job loss, family anxiety, and numerous other harms caused by access barriers.
Implications and Opportunities from the Recent Children’s Behavioral Health Class-Action Lawsuit
In August of 2025, New York State settled a class-action lawsuit requiring New York to develop and implement a multi-year plan to provide timely access to intensive home and community-based mental health services statewide to children in Medicaid. The findings that resulted in this settlement reaffirm the long-standing experiences of children, youth, and families throughout the state who have struggled to access comprehensive, timely home and community-based services.
CCC believes this settlement could offer an opportunity to transform New York’s behavioral health system into one that meets the needs of all children and families across the state. The Settlement requires significant system reforms aimed at improving behavioral health access, improving child outcomes, and reducing unnecessary admissions to psychiatric hospitals, emergency departments, psychiatric residential treatment facilities, or other congregate settings. The Settlement also includes requirements for robust stakeholder involvement, data transparency, and impact monitoring.
Among the provisions of the settlement are requirements that the State’s Implementation plan include proposed reimbursement rates for each relevant service “set at amounts to ensure that payments to providers are consistent with efficiency, economy, and quality care and are sufficient to enlist enough providers to meet the needs of eligible children on a timely basis in all regions and areas of New York State, at least to the extent that they are available to the general population in the geographic area. There shall be a reasonable and sound basis for any models or analyses used to determine reimbursement rates, and for all assumptions used in connection with such models or analysis.” The settlement agreement also requires that the State conduct a regular review of reimbursement rates to determine whether rates constitute a barrier to access requiring corrective action.
Collectively, these mandated reforms can put New York State on a path towards addressing the severe access barriers facing thousands of families across the state.
Recommendations
1. Invest $200 million to increase access to children’s behavioral health outpatient services.
For years, CCC and the HMHK campaign has drawn attention to the lack of access to a continuum of adequate behavioral services and supports for children, and in particular the lack of adequate outpatient services. The class-action settlement reaffirms the urgent need to reform the system, and mandates rate reforms as part of the strategies New York must include in its implementation plan.
Since 2023, the Healthy Minds, Healthy Kids Campaign has recommended an investment of $200 million to shore up Article 31 clinic, Article 32 clinic, CFTSS, and HCBS rates (these reforms are also addressed in A.8600 (Simon)/S.8427 (Brouk)). This proposal is based on a first-of-its-kind study of reforms needed to address rate inadequacy and workforce shortages, and is estimated to add 1,300 additional professionals to the workforce and serve over 26,000 additional children. This rate reform proposal directly addresses the CFTSS and HCBS services targeted in the state settlement, but also uplifts the urgency of addressing clinical Article 31 and Article 32 services in conjunction with home and community-based services.
New York must move with urgency to implement rate reforms we know are needed to strengthen and expand the children’s behavioral health workforce, and combat the chronic waitlist crisis. As the State is considering solutions to meet the requirements of the settlement, we urge the State to act with haste to fund and implement these proposed reforms:
Trend rates to keep pace with inflation
Trends maintain, but do not advance, the children’s behavioral health delivery system
- 2% trend for children’s behavioral health clinic services: $10,749,230
- 2% trend for children’s HCBS and CFTSS services: $2,107,748
Establish a care team coordination fee
Providers are responsible for coordinating with a growing array of care managers. They should be compensated for the time it takes to do so.
- $7.50 Per Served Member Per Month (PSMPM) fee for children’s clinics: $12,112,200
- $7.50 PSMPM for CFTSS and children’s HCBS: $8,324,766
Adjust children’s clinic rates to reflect the unique and complex care children require
Account for the additional costs of navigating the complex web of service systems children and their families are at the nexus of. Enable providers to expand their capacity to meet the need.
- 35% enhancement for clinic visits provided to children: $117,569,701
Adjust CFTSS and children’s HCBS to account for realistic volume for home and community-based services
Enable providers to expand capacity by acknowledging that the anticipated volume efficiencies have not materialized.
- Increase in CFTSS and children’s HCBS rates to reflect the lack of economies of scale: $44,460,329
Total investment in children’s behavioral health: $200 million
2. Carve mental health and substance use disorder services out of Medicaid managed care.
Since 2019, for-profit managed care companies have been responsible for managing Medicaid mental health and substance use disorder supports for children in the State. In that time, it has become clear that the managed care system has failed New York’s children:
- Youth suicide rates in NYS have risen by nearly 10% since 2014, and providers across the state report widespread waitlists and delayed care for children’s services.[iii]
- In an effort to contain costs, managed care companies regularly deny claims for care, delay payments, and introduce onerous administrative barriers that harm access to care.
- Each year managed care companies in NYS make approximately $400 million in profits that could instead be reinvested into behavioral health services for New Yorkers.
It is past time that New York reject a system that creates new barriers for families while generating profits for managed care companies. We join the NYS Council for Community Behavioral Health Care and advocates across the state in urging New York leaders to remove OMH and OASAS community-based behavioral health (mental health and substance use) services, including outpatient, residential, and rehabilitation services, from the state’s Medicaid managed care program [S.8309A (Brouk)/A.8055 (Simon)].
Carving behavioral health services out of managed care will improve access for children and families by allowing hundreds of millions of dollars can be reinvested into providing services rather than providing profits for managed care companies. Providers will face fewer administrative barriers, denials, and delays, allowing them to provide higher quality care and reduce waitlists for services.
Conclusion
All children and families with mental health and substance use disorder needs deserve to be met with timely, high-quality care. Through targeted investments in the children’s outpatient system, New York can begin to redress the underlying inequities that led to the recent class action lawsuit with the State.
We again thank the Chairs members of the Committee for holding today’s hearing, and look forward to continued work on these urgent issues.


